Fatty liver disease is one of the fastest-growing health concerns worldwide, impacting roughly 32% of people worldwide, according to a 2022 systematic review. It is closely tied to rising rates of obesity, diabetes, and metabolic dysfunction. However, recent research highlights another possible contributor that often goes unnoticed: vitamin D deficiency.
Could maintaining optimal vitamin D levels help protect the liver? Here’s what the evidence suggests.
What Is Fatty Liver Disease?
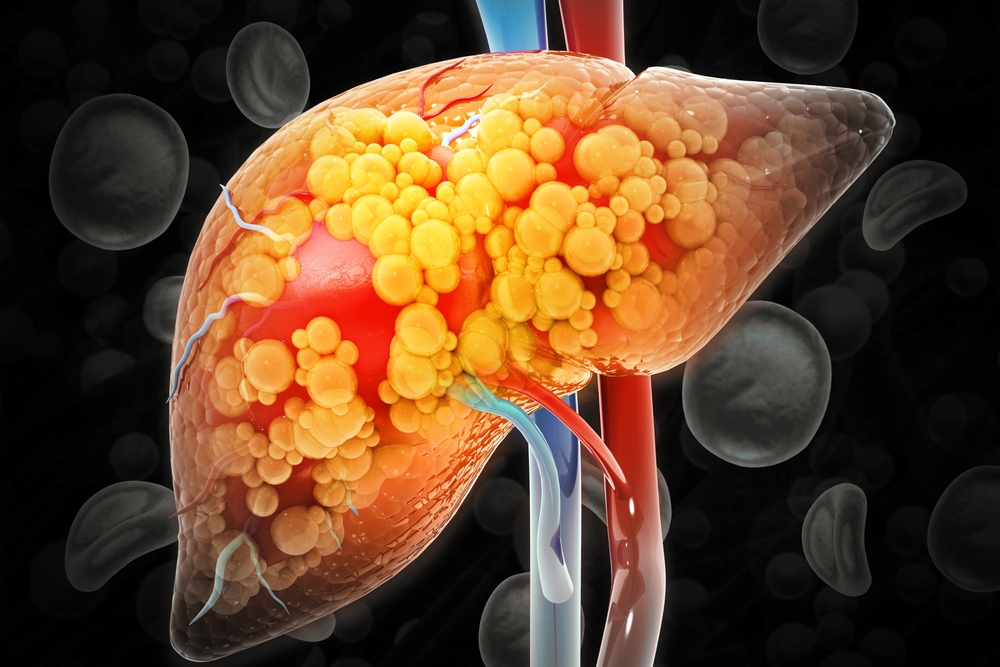
Fatty liver disease (FLD), or hepatic steatosis, occurs when excess fat accumulates in the liver. While early stages are often silent, persistent fat buildup can impair liver function and lead to serious complications, including inflammation, fibrosis, cirrhosis, and in some cases, liver cancer.
There are two primary types of fatty liver disease:
1. Metabolic Dysfunction–Associated Steatotic Liver Disease (MASLD)
Previously known as non-alcoholic fatty liver disease (NAFLD), MASLD affects approximately 1 in 3 U.S. adults according to WebMD. It develops in individuals with underlying metabolic risk factors such as:
- Obesity
- Type 2 diabetes
- Insulin resistance
- High blood pressure
- Elevated cholesterol or triglycerides
MASLD includes two forms:
- Simple steatosis: Fat accumulation without significant inflammation or liver damage.
- MASH (Metabolic dysfunction–associated steatohepatitis): A more advanced form involving inflammation and hepatocellular injury. MASH can progress to fibrosis, cirrhosis, and even hepatocellular carcinoma. About 20% of individuals with MASLD develop MASH, reports WebMD.
2. Alcohol-Related Liver Disease (ALD)
This form results from excessive alcohol consumption and affects roughly 5% of U.S. adults. While early-stage ALD can be reversible with abstinence, continued alcohol use increases the risk of liver inflammation, fibrosis, and long-term liver damage.
The Role of Vitamin D in Liver Health

Vitamin D is essential not only for bone metabolism but also for immune function, inflammation control, insulin sensitivity, and cellular health, all of which are highly relevant to liver function.
Once produced in the skin through sunlight exposure or obtained from food/supplements, vitamin D is first converted in the liver to 25-hydroxyvitamin D [25(OH)D], then activated by the kidneys into its biologically active form.
Key ways vitamin D supports liver health include:
- Improving metabolic function: Enhances insulin sensitivity and helps regulate glucose and lipid metabolism in liver cells
- Reducing liver inflammation: Suppresses pro-inflammatory cytokines and promotes immune balance
- Inhibiting fibrosis: Helps reduce collagen buildup and fibrotic activity, potentially slowing the development of liver scarring
- Strengthening immune defenses: Supports the liver’s role in defending against toxins and microbial threats
Vitamin D Deficiency and Its Association with MASLD
Growing evidence links low vitamin D levels with an increased risk of MASLD and more severe liver disease.
One large cross-sectional study of over 22,000 individuals found a strong correlation between low vitamin D and higher risk of MASLD, independent of gender or other metabolic risk factors.
Other studies have reported that:
- Individuals with MASLD are significantly more likely to be vitamin D deficient
- Lower vitamin D levels are associated with increased liver fat, greater inflammation, and higher fibrosis scores on biopsy
- A pooled analysis estimated that people with MASLD are 1.26 times more likely to have low vitamin D compared to those without the condition
While the association is strong and biologically plausible, more research is needed to confirm whether low vitamin D directly causes liver disease or simply reflects broader metabolic dysfunction.
Can Vitamin D Supplementation Help?

Emerging clinical trials suggest that vitamin D supplementation may benefit individuals with MASLD by improving:
- Liver enzymes, particularly ALT (alanine aminotransferase)
- Insulin sensitivity
- Lipid profiles, such as increasing HDL cholesterol
- Body composition, including reductions in weight or waist circumference
However, vitamin D should be viewed as a complementary therapy, not a standalone treatment. The best results are typically seen when supplementation is combined with lifestyle changes like:
- Weight loss
- Physical activity
- Dietary improvements
What Can You Do?

If you’re concerned about your liver health, or your vitamin D status, here are practical steps to take:
- Get tested: A simple blood test can measure your vitamin D levels.
- Consider safe sun exposure: Short, regular exposure to sunlight helps your body produce vitamin D naturally.
- Eat vitamin D-rich foods: Such as fatty fish (salmon, tuna), fortified dairy, egg yolks, and mushrooms.
- Talk to your healthcare provider: They can guide you on whether supplementation is needed and how much to take.
Final Thoughts

Vitamin D plays an often-overlooked but important role in maintaining liver health. Low levels of vitamin D are common in people with MASLD and may contribute to worsening liver inflammation, fibrosis, and metabolic dysfunction.
Although more research is needed to fully understand the relationship, maintaining adequate vitamin D levels, through sunlight, diet, or supplements, may offer a simple strategy to support liver function and reduce fatty liver disease risk.
If you’re at risk for MASLD or vitamin D deficiency, consult your healthcare provider about evaluation and next steps.
Disclaimer: This information is not intended to be a substitute for professional medical advice, diagnosis or treatment and is for information only. Always seek the advice of your physician or another qualified health provider with any questions about your medical condition and/or current medication. Do not disregard professional medical advice or delay seeking advice or treatment because of something you have read here.
Read More: How to Support Liver Health in Your 50s, 60s, and Beyond
