When we think of cancer risk, factors like smoking, sun exposure, or family history often spring to mind, while these are certainly important, the single most significant risk factor for developing cancer is something none of us can avoid: aging.
The incidence of cancer rises dramatically with age. In fact, most cancers are diagnosed in people aged 65 and older. But why is this the case? The science points to a complex interplay between the accumulation of damage over a lifetime and the gradual breakdown of the body’s defenses.
The Science of Aging and Cancer Risk
Aging is inevitable, and while it is often spoken about negatively, truly aging is a gift. Not everyone gets the opportunity to get older. That being said, the older we get, the more this becomes our number one risk factor for cancer. The increased risk of cancer with age isn’t due to a single process, but rather a perfect storm of biological changes that occur over decades.
1. Accumulation of DNA Damage and Mutations
Image credit: Shutterstock
Every cell in your body is constantly exposed to factors that can damage its DNA. This includes environmental toxins, radiation, and even normal byproducts of metabolism (like reactive oxygen species). The older we get, the longer our cells have been exposed to these damaging agents. This leads to a greater number of accumulated mutations in our DNA. Cancer then arises when mutations occur in critical genes, specifically oncogenes. And tumor suppressor genes. Oncogenes promote growth, while tumor suppressor genes restrict it. The more opportunities for mutation, the higher the chance of hitting these critical targets.
2. Cellular Senescence and the “Senescence-Associated Secretory Phenotype (SASP)”
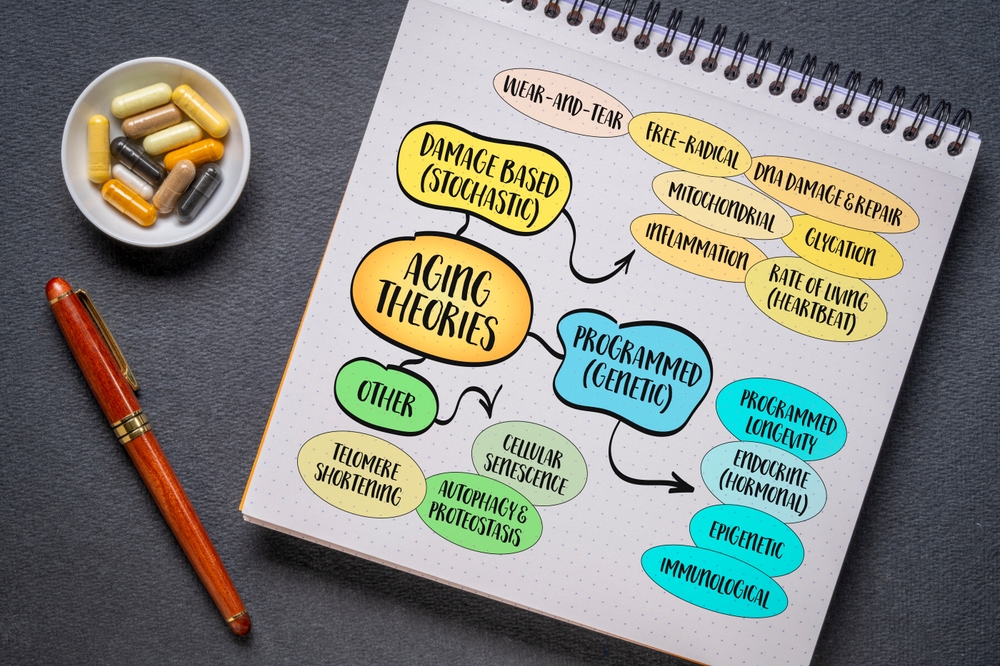
As cells age, some enter a state called senescence, where they stop dividing but remain metabolically active. While senescence initially evolved as a protective mechanism against cancer, by stopping potentially cancerous cells from dividing, senescent cells eventually become detrimental. This is for a couple of reasons.
First, senescent cells release a cocktail of pro-inflammatory signals, growth factors, and enzymes called the SASP. Next, the SASP creates a pro-inflammatory microenvironment in the surrounding tissue. This inflammation provides the perfect conditions, like fertile soil for tumor growth or what is called a ‘cancer niche’, for nearby mutated cells to survive, proliferate, and become a malignant tumor.
3. Immunosenescence (Weakened Immune Surveillance)

Image credit: Shutterstock
Your immune system is a powerful cancer surveillance system. It is constantly identifying and destroying abnormal cells before they can form a tumor. With age, the immune system undergoes a decline in function. This is a process called immunosenescence. Essentially, your immune system becomes less effective. Immune cells, particularly T-cells, become less capable at recognizing and eliminating cancer cells. This weakened surveillance allows nascent tumors to “escape” detection and grow unchecked.
Addressing Ageism and Specialized Care

Image credit: Shutterstock
Despite aging being the leading risk factor, the standard medical approach to cancer treatment often overlooks the specific needs of older patients. This gap is often exacerbated by ageism in healthcare.
Ageism in Healthcare

Image credit: Shutterstock
The first hurdle is under-treatment. Older patients are often offered less aggressive or sub-optimal treatments based on assumptions about their tolerance or life expectancy, rather than a rigorous assessment of their functional status and overall health (also known as comorbidity). The second is that, despite being the highest risk for developing cancer, they are often excluded from clinical trials. Historically, older adults, especially those with multiple health issues, have been underrepresented in cancer clinical trials. This has led to a lack of evidence-based guidelines for this patient population.
The Importance of Geriatric Oncology Clinics

Image credit: Shutterstock
Specialized geriatric oncology clinics are essential to provide optimal care. They shift the focus from a patient’s chronological age to their biological age and overall resilience. These clinics often employ a Comprehensive Geriatric Assessment (CGA). This is a crucial tool that looks beyond the cancer diagnosis to evaluate factors like nutritional status, cognitive function, social support, and existing health conditions. Geriatric oncology clinics also provide a more personalized treatment based on the results of the CGA. This means doctors can adjust chemotherapy doses, incorporate physical therapy, or manage drug interactions to maximize effectiveness while minimizing debilitating side effects. The goal is to treat the cancer aggressively while maintaining the patient’s quality of life and independence.
Special Focus: Comprehensive Geriatric Assessment (CGA)

Image credit: Shutterstock
For older adults, where the risk of cancer is highest, specialized care is vital to determine the most appropriate treatment. The CGA is a multidimensional, multidisciplinary diagnostic process used to evaluate an older person’s medical, psychosocial, and functional capabilities and limitations. It moves beyond a patient’s chronological age and cancer diagnosis to provide a holistic view of their health. The CGA typically evaluates:
- Functional Status: The ability to perform daily activities (walking, dressing, etc).
- Comorbidities: The presence and severity of other existing health conditions.
- Cognitive and Psychological Health: Screening for issues like depression and cognitive impairment.
- Nutritional Status: Assessing for weight loss or malnutrition.
- Social Support: Evaluating the patient’s living situation and support network.
The results of the CGA are then used by the oncology team to make personalized decisions regarding cancer therapy, such as adjusting chemotherapy doses, recommending supportive care, or incorporating specialized physical therapy, to ensure treatment maximizes the change of cure or remission while preserving the patient’s independence and quality of life.
Factors You Can Control to Reduce Risk

Image credit: Shutterstock
While aging is inevitable, cancer risk is not solely determined by it. It’s vital to understand that a significant portion of cancer cases are linked to preventable risk factors. Focusing on these allows individuals to take control of their health trajectory.
The risk of developing cancer is influenced by a combination of factors, some that are outside of our control and many that we can actively manage. While aging is the most significant, unavoidable risk factor, a substantial portion of cancer cases are linked to preventable lifestyle and environmental exposures.
Controllable Risk Factors and Reduction Strategies

Individuals can significantly lower their personal cancer risk by focusing on several key areas. Tobacco use is a major preventable cause of cancer. The simplest strategy to mitigate this risk is to avoid all forms of tobacco and exposure to secondhand smoke. Maintaining a healthy diet and weight is also crucial; this involves achieving and maintaining a healthy body weight, consuming a diet rich in whole grains, fruits, and vegetables, and limiting intake of red and processed meats.
Furthermore, engaging in physical activity regularly, at a moderate to vigorous intensity, helps reduce risk. Limiting or avoiding alcohol consumption also plays a role in prevention. To protect against skin cancers, people should limit sun and UV exposure by using broad-spectrum sunscreen, wearing protective clothing, and seeking shade, especially during peak sunlight hours. Finally, the risk of some cancers linked to chronic infections can be managed by getting vaccinated against viruses such as Human Papillomavirus (HPV) and Hepatitis B, and by limiting environmental exposure to known carcinogens like asbestos and radon.
Mastering the Balance of Risk

Image credit: Shutterstock
The conversation around cancer risk must fundamentally acknowledge that aging is the primary, uncontrollable driver of incidence. The steady accumulation of DNA damage, the chronic inflammation fostered by senescent cells, and the decline of the immune system (immunosenescence) all converge to make the later decades of life the most vulnerable period.
However, this scientific reality is not a sentence of inevitability. While we cannot stop the clock, we can actively manage the other significant variables. The single most powerful action an individual can take is to control the modifiable factors. This means avoiding tobacco, maintaining a healthy weight, exercising regularly, and utilizing preventative measures like vaccinations.
For those who do face a cancer diagnosis in later life, the push for personalized, age-attuned care, guided by the CGA, is critical. By treating the whole person, not just the tumor, healthcare providers can ensure that older adults receive effective treatment that preserves their function and quality of life. Ultimately, understanding cancer risk is about mastering this balance: accepting the unavoidable risk of time, while vigorously pursuing the controllable gains of healthy living and specialized care. This combined approach offers the best defense in the enduring fight against cancer.
Disclaimer: This information is not intended to be a substitute for professional medical advice, diagnosis or treatment and is for information only. Always seek the advice of your physician or another qualified health provider with any questions about your medical condition and/or current medication. Do not disregard professional medical advice or delay seeking advice or treatment because of something you have read here.
Read More: These Foods Could Be Fueling the Surge in Early-Onset Colorectal Cancer Among Women
