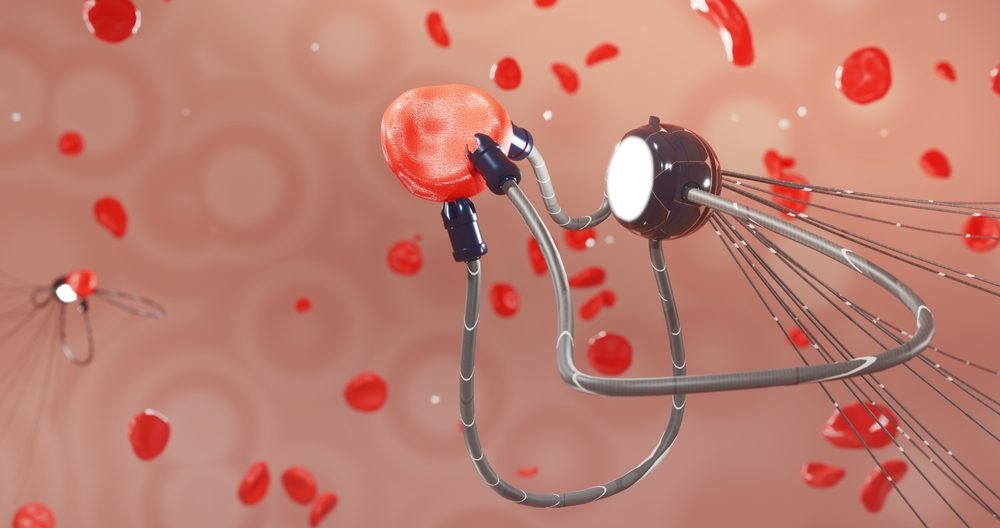
In the world of biomechanics and medicine, there are challenges in the designing microrobots that are effective in drug administration. Properly managing factors such as biocompatibility, size, biodegradability, and magnetic properties is required to control the microrobots effectively. Researchers at ETH Zurich have developed a microrobot that promises to revolutionize medicine delivery inside the body.
The research team has reported that the microrobot can transport various medications directly through blood vessels to diseased tissue. It then dissolves and releases the medication at its target. The design of the microrobotic system combines electromagnetic navigation, a release catheter, and dissolvable drug-loaded capsules. It also marks a pivotal achievement in medical robotics. These microbots could potentially revolutionize the treatment of strokes, tumors, and localized infections with incredible precision.
An estimated 12 million people worldwide suffer a stroke every year, with many dying or becoming permanently disabled. Current stroke treatments require high doses of medication that spread throughout the entire body. This approach often causes severe side effects, including dangerous internal bleeding. The ETH Zurich microbots offer a promising alternative by delivering medication precisely where it is needed.
The Problem With Traditional Drug Delivery Methods
Current methods of treatment for strokes require administering a high dosage of drugs that are either injected or taken in pill form and spread throughout the body. The drugs eventually dissolve the thrombus that blocks the blood vessel. The current methods of drug delivery face significant limitations that reduce their effectiveness and safety. Only a tiny fraction of the drug actually reaches the target site, forcing doctors to prescribe higher doses. This systemic distribution exposes healthy tissues and organs to potentially harmful substances.
A current and pressing example of harmful treatments that would benefit from this technology is Chemotherapy. Chemotherapy drugs target rapidly dividing cells, including both cancerous and healthy ones. Patients frequently experience devastating side effects, including hair loss, nausea, fatigue, and organ damage. The blood-brain barrier poses another formidable challenge to effective treatment of neurological conditions. More than 98% of small-molecule drugs and nearly all large-molecule medicines are not able to pass beyond this protective membrane.
Thrombolytic therapy for stroke patients requires doctors to administer powerful blood-thinning medication that spreads through the entire circulatory system. About 5% of patients who receive thrombolytic therapy experience major bleeding complications. Approximately 1% suffer brain bleeds that cause additional strokes, turning a treatment into a potential danger.
ETH Zurich’s Revolutionary Microrobot Technology

Researchers at ETH Zurich have developed a magnetically guided microrobot capable of precise navigation under clinical conditions. The microrobot comprises a proprietary spherical capsule made of a soluble gel shell loaded with medication. Iron oxide nanoparticles embedded in the capsule provide the magnetic properties necessary for external control. This innovative design allows doctors to guide the tiny device through complex blood vessel networks to specific targets.
Lead author Fabian Landers, a postdoctoral researcher at the Multi-Scale Robotics Lab at ETH Zurich, explained the engineering challenge involved. “Because the vessels in the human brain are so small, there is a limit to how big the capsule can be,” Landers said. The researchers needed to ensure that such a small capsule still possessed sufficient magnetic properties for reliable control.
The microrobots also require a contrast agent that enables X-ray tracking. This would allow doctors to actively view and navigate the microrobot through the blood vessels. Researchers looked at tantalum nanoparticles, which are used in medical applications. However, these nanoparticles have a greater density and weight, which makes navigating them difficult.
Professor Bradley Nelson has researched microrobots at ETH Zurich and explained that “Combining magnetic functionality, imaging visibility and precise control in a single microrobot required perfect synergy between materials science and robotics engineering”. Professor Salvador Pané’s team developed precision iron oxide nanoparticles that were fundamental to the project.
How the Microbot Navigation System Works
The researchers developed an ingenious 2-step strategy to bring the microrobot close to its target destination. First, they inject the microbot into the blood or cerebrospinal fluid through a specially designed catheter. The catheter uses a commercially available design modified with an internal guidewire connected to a flexible polymer gripper. When pushed beyond the external guide, the polymer gripper opens and releases the microrobot into the bloodstream.
The electromagnetic navigation system then takes over to guide the microrobot to its exact destination. “The speed of blood flow in the human arterial system varies a lot depending on location,” Nelson explained. This variability makes navigating a microbot extremely complex, requiring sophisticated control systems and strategies.
The team combined three different magnetic navigation strategies to achieve reliable control in all vessel types. The first strategy rolls the capsule along the vessel wall using a rotating magnetic field at 4 millimeters per second. The second strategy uses magnetic field gradients to pull the microbot through the vessel toward stronger fields. The microrobot can even travel against blood flow velocities exceeding 20 centimeters per second using this technique.
Precision Delivery at Blood Vessel Junctions
When the microrobot reaches complex junctions where vessels branch in multiple directions, in-flow navigation is activated. The magnetic gradient is directed against the vessel wall, thereby carrying the capsule into the correct vessel. This sophisticated approach allows precise navigation even at the most challenging anatomical locations in the brain.
By integrating these 3 navigation strategies, the researchers achieved effective control across a range of flow conditions. In more than 95% of the cases tested, the capsule successfully delivered the drug to the correct location. “Magnetic fields and gradients are ideal for minimally invasive procedures because they penetrate deep into the body,” Nelson explained.
Landers expressed amazement at the challenges posed by human blood flow dynamics. “It’s remarkable how much blood flows through our vessels and at such high speed,” he said. The navigation system must withstand tremendous forces while maintaining precise control over the small microrobot.
Drug Loading and Release Mechanism
The microrobots contain the active pharmaceutical drugs needed for each specific medical application. Researchers successfully loaded the microrobots with common drugs for various applications during testing. These included thrombolytic agents for stroke, antibiotics for infections, and anticancer agents for cancer treatment.
The drug-release mechanism employs controlled heating to dissolve the gel shell at the target site. A high-frequency magnetic field heats the magnetic nanoparticles embedded within the capsule. This heating dissolves the gel shell and releases the medication precisely where needed. The microbot completely dissolves, leaving no foreign material in the patient.
Realistic Testing and Animal Trials

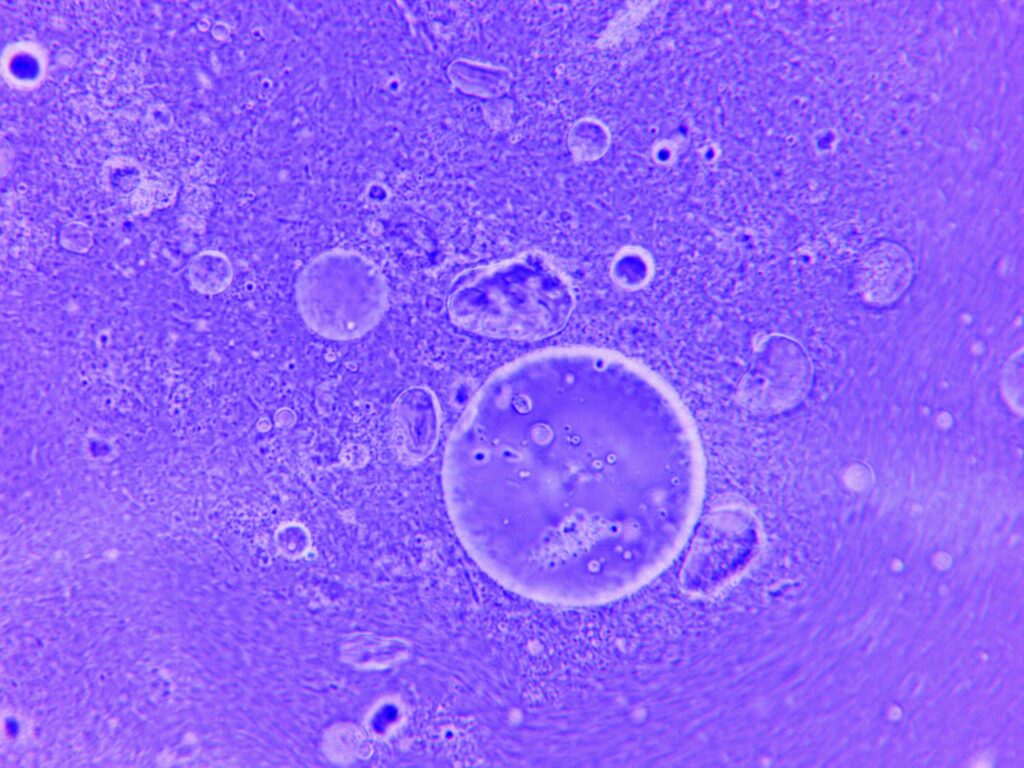
The research team developed innovative silicone models to test their microrobots in realistic clinical environments. These models accurately replicate the blood vessels of human patients and animals. The vessel models proved so realistic that they are now used in medical training programs across the globe. ETH spin-off company Swiss Vascular now manufactures and markets these models commercially.
“The models are crucial for us, as we practised extensively to optimise the strategy and its components,” explained Pané. Animal experimentation presents ethical concerns and practical limitations that the silicone models help researchers avoid. In the models, researchers successfully targeted and completely dissolved simulated blood clots.
After numerous successful trials in the silicone models, the team tested their microbots under real clinical conditions. They demonstrated in pigs that all three navigation methods work, and the microrobot remains clearly visible throughout procedures. The researchers also navigated microrobots through the cerebrospinal fluid of sheep successfully.
Successful Large Animal Demonstrations

The animal trials confirmed the microrobot platform’s viability for future human clinical trials. The porcine model validated all locomotion strategies under clinical conditions with precise cerebrovascular navigation. The ovine model demonstrated the platform’s ability to operate within anatomically constrained central nervous system regions.
Landers expressed excitement about the cerebrospinal fluid navigation results specifically. “This complex anatomical environment has enormous potential for further therapeutic interventions,” he said. The successful navigation in this challenging environment opens doors for treating conditions beyond vascular occlusions.
The international study involved researchers beyond ETH Zurich, including Professor Josep Puigmartí-Luis from the University of Barcelona. The collaboration emerged from the European ANGIE project coordinated by Professor Salvador Pané at ETH Zurich. This international cooperation combined expertise in chemistry, materials science, and robotics engineering.
FDA-Approved Materials and Safety Considerations

The researchers specifically designed their microrobot platform with regulatory approval and clinical safety in mind. The system uses biocompatible materials already approved by the United States Food and Drug Administration. Iron oxide nanoparticles have received FDA approval for various medical applications, including cancer treatment and imaging.
“The new system overcomes major clinical barriers through precise and safe electromagnetic control,” explained Puigmartí-Luis. The microbots navigate the body without direct physical contact with the vessel walls during most of their journey. Real-time imaging ensures stable, safe, and adaptable handling in real medical environments throughout procedures.
The platform integrates a clinical electromagnetic navigation system called Navion with custom-designed components. This integration allows the technology to fit seamlessly into existing hospital operating room infrastructure. The modular design means hospitals could adopt the technology without completely overhauling their current equipment.
Applications Beyond Stroke Treatment
Credit: Shutterstock
While stroke treatment represents the most immediately promising application, the microrobots have far broader potential. Researchers successfully loaded the capsules with antibiotics for treating localized infections deep within the body. Tumor medications could deliver chemotherapy directly to cancer cells while sparing healthy tissue.
The precision drug delivery approach could dramatically reduce the side effects associated with cancer treatment. Current chemotherapy affects rapidly dividing healthy cells throughout the body, causing hair loss and immune suppression. Microrobot delivery could concentrate toxic drugs precisely at tumor sites, minimizing collateral damage to healthy tissues.
Interventional radiologists see potential for combining microbots with existing imaging systems in exciting new ways. Real-time tracking under X-ray or MRI control could enable procedures currently requiring complex catheter navigation. Procedures previously considered impossible, such as reaching extremely small branching vessels, may become routine.
The Road to Human Clinical Trials

The ETH Zurich research team maintains laser focus on bringing its technology to hospital operating rooms quickly. At every stage of development, the team prioritized ensuring clinical readiness for real medical applications. The next goal involves beginning human clinical trials as soon as regulatory approvals allow.
Most experts believe human trials for microrobot drug delivery will begin within the next few years. Early studies will likely focus on drug delivery in controlled environments like the bladder or stomach. These locations offer more manageable conditions compared to the complexity of the entire circulatory system.
Landers spoke passionately about the team’s motivation for pushing this technology forward so aggressively. “Doctors are already doing an incredible job in hospitals,” he acknowledged. “What drives us is the knowledge that we have a technology that enables us to help patients faster and more effectively.”
Challenges and Limitations Ahead
Despite remarkable progress, significant challenges remain before microbots become standard medical practice. Navigation in living environments remains complex due to unpredictable blood flow and tissue resistance. Individual patient anatomy varies considerably, requiring adaptive control systems for reliable operation.
Red blood cells present obstacles for microbots navigating through blood vessels at microscopic scales. These concentrated cells can trap or deflect microbots from their intended paths during navigation. The pulsatile nature of blood flow from the heart cycle adds another layer of complexity.
Regulatory agencies will need to classify microbots appropriately for approval and oversight purposes. Safety testing must be thorough, especially for devices intended to remain in the body during procedures. Integration with existing hospital imaging systems without affecting their performance requires additional engineering work.
Read More: World’s Smallest Pacemaker, the Size of a Rice Grain, Marks Major Medical Breakthrough
The Broader Microrobot Research Landscape

ETH Zurich’s breakthrough builds upon decades of microrobot research happening at institutions worldwide. Purdue University researchers developed a magnetic microdevice that removes blood accumulating during hemorrhagic strokes. Their innovation achieved 86 percent effectiveness in animal models for clearing blood from the brain ventricles.
Artedrone’s SASHA system uses autonomous magnetic microbots for mechanical thrombectomy procedures in stroke patients. Their preclinical studies tested the system in human cerebral vasculature models and porcine brain anatomy. The goal involves enabling non-specialist clinicians to perform advanced stroke interventions at more hospitals.
Microrobot Medical recently received FDA 510(k) clearance for its LIBERTY endovascular robotic system. This clearance positions the company to commercialize the first FDA-cleared single-use remotely operated robotic system. The pivotal study demonstrated 100% success in robotic navigation to designated targets, with no device-related adverse events.
Conclusion
The ETH Zurich microbot represents a potential paradigm shift in how medicine reaches diseased tissue inside the human body. By delivering drugs directly to their targets, microbots could dramatically reduce the side effects plaguing current treatment approaches. The technology has demonstrated remarkable success rates exceeding 95 percent in animal trials under clinical conditions.
Given that millions of people suffer strokes annually and countless others endure chemotherapy’s side effects, the stakes could not be higher. The international research team has prioritized clinical readiness throughout development, using FDA-approved biocompatible materials. Human clinical trials may begin within the next few years as the technology continues to advance rapidly.
The convergence of robotics, materials science, and medical imaging has made science fiction into an emerging medical reality. These microscopic machines navigating through blood vessels may soon become as routine as the pills and injections they could replace. Your next prescription might not come in a bottle; it might swim directly to where your body needs it most.
Disclaimer: This article was created with AI assistance and edited by a human for accuracy and clarity.
Read More: The Story of Henrietta Lacks: How a Medical Miracle Was Born from Injustice
