This site contains product affiliate links. We may receive a commission if you make a purchase after clicking on one of these links
That burning feeling when you pee, the constant urge to run to the bathroom, and that sinking dread when you realize what’s happening. If you’re a woman, you’ll likely face a urinary tract infection (UTI) at some point. Many deal with them repeatedly, disrupting work, relationships, and daily life. Here’s what you need to know about recognizing, treating, and preventing this common condition at every stage of your life, and practical steps that work.
What Is a UTI?
Urinary tract infections develop when bacteria enter the urinary system and multiply. Half of all women will experience one at least once in their lifetime. The culprit behind this is E. coli, a type of bacteria that normally lives harmlessly in the intestines. When this bacterium reaches your urinary tract, it multiplies and causes problems. About 85% happen this way. While the bacteria usually stay in your bladder, germs that reach your kidneys create a much more serious situation.
Recognizing the Symptoms
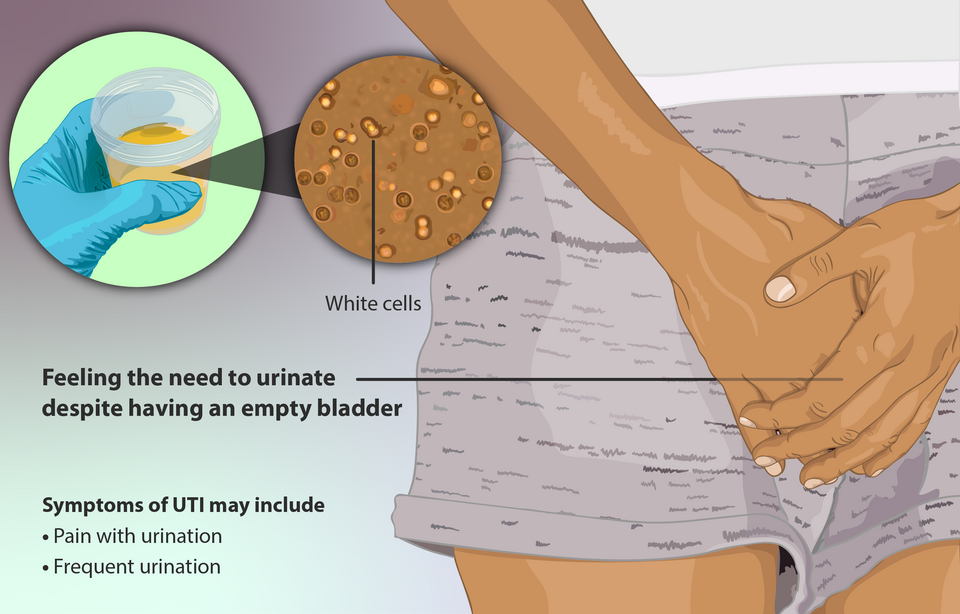
The most common is a burning sensation when you pee, along with feeling like you need to go constantly, even when little comes out. Your urine may also look cloudy or bloody and smell stronger than usual. The pain can vary from sharp burning during urination to a dull ache in your lower belly. You might feel that urgent need to pee even right after you’ve just used the bathroom.
Read More: 5 Major Feminine Hygiene Mistakes That Can Affect Women’s Health
Why Women Are More Vulnerable
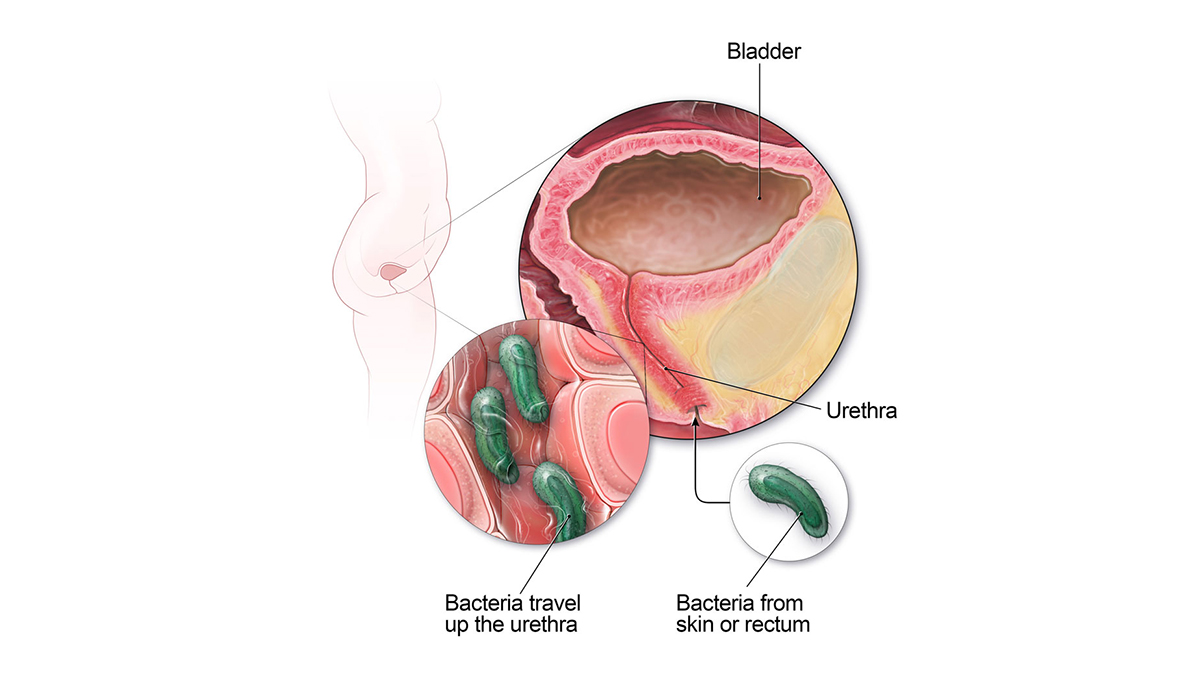
UTIs in women occur about 30 times more often than in men. A woman’s urethra spans only about 1.5 inches. Men’s urethras are about 8 inches long. The urethra opening also sits close to the vagina and rectum, where bacteria naturally live. This short distance creates problems during normal activities like wiping after using the bathroom or having sex. Bacteria can easily travel to the urethra and quickly reach your bladder before your body has time to flush them out.
Sexual Activity and Bacterial Risk

Given this anatomical vulnerability, it’s no surprise that sex pushes bacteria toward the urethra and into the bladder. Some women develop bladder infections every time they’re sexually active, a pattern called honeymoon cystitis. The timing is so predictable that many women can link them directly to sexual activity within 24 to 48 hours. Using unlubricated condoms can make this worse by creating additional friction and irritation.
Read More: How a Lack of Alone Time Affects the Mental Health of Moms
Hormones and Your Cycle

The female hormone estrogen supports protective bacteria that defend against harmful germs. When estrogen drops during periods, after menopause, or while breastfeeding, women lose this natural protection. This explains why some women notice these infections cluster around their menstrual cycle. During menstruation, hormone changes and pH shifts in the vagina can disrupt the balance of protective bacteria. This increases your infection risk in the days before or during periods.
Birth Control and Other Risk Factors

Spermicides and diaphragms raise your risk because they irritate tissues and disrupt natural bacteria. On the other hand, hormone-based birth control methods may help by supporting natural defenses through consistent estrogen levels. Beyond contraception, several health conditions and life changes affect risk.
Pregnancy brings hormonal shifts and physical pressure on the bladder that makes it harder to empty. Diabetes weakens the immune response while creating higher sugar levels in urine that bacteria can feed on. These often come back because bacteria can hide in bladder tissues and emerge later, even after treatment.
Getting an Accurate Diagnosis

When you think you might have one, proper testing confirms what’s happening and ensures the right treatment. Healthcare providers will ask for a clean urine sample to check for bacteria and white blood cells, which are the body’s germ fighters. Getting an accurate sample requires following a specific collection method.
Providers recommend cleaning the genital area with the provided wipe. Start to urinate, then catch the middle part of the stream in the cup. This technique avoids contamination from skin bacteria that could create false results. The good news is that doctors have updated their diagnostic standards, so you don’t need to wait as long for answers. They now know that 1,000 bacteria, along with symptoms, usually means infection, rather than the old requirement of 100,000 bacteria.
Read More: The Long-Overdue Research on Women’s Bodies: What Scientists Are Discovering
Antibiotic Treatment That Works

Once doctors confirm the infection, they’ll prescribe proven antibiotics that work best against the bacteria involved. These newer antibiotics work better than older ones like amoxicillin and ampicillin because bacteria have developed resistance to the older drugs. Research shows that up to 40% of bladder infections can be cleared with increased water intake and pain relief medications like ibuprofen. Your doctor may suggest starting with these approaches for mild symptoms while waiting for test results.
When antibiotics are needed, taking the full course is essential, even when you start feeling better after a day or two.Stopping early can lead to antibiotic resistance and make future bladder infections harder to treat. Never share antibiotics with others, and call your doctor if symptoms don’t improve within 2 to 3 days or start getting worse.
Warning Signs for Emergency Care

Watch for serious warning signs that mean bacteria have spread beyond your bladder. Fever over 101°F, severe back or side pain, nausea, vomiting, or confusion in elderly people are all red flags. These suggest bacteria have reached your kidneys or entered your bloodstream, creating a dangerous condition called sepsis.
If you develop any fever or symptoms persist beyond a day, see a doctor because antibiotic therapy can be crucial for stopping bacteria from reaching your kidneys. When serious symptoms appear, you need immediate medical attention because kidney infections can cause permanent damage and require intravenous antibiotics. Seek emergency medical care within hours, not days.
Daily Prevention Habits

Drinking water serves as one of your best defenses in how to prevent UTIs by helping flush bacteria before they multiply. An extra 6 cups daily can cut infection risk in half by creating more frequent urination that sweeps bacteria out of your urinary tract. Aim for pale yellow urine and urinating every 2 to 3 hours during the day.
Don’t hold urine when you feel the urge, as this gives bacteria more time to multiply in your bladder. Beyond hydration, your bathroom routine plays a key role in prevention. Always wipe from front to back after using the bathroom to keep intestinal bacteria away from your urethra. This simple habit stops the main way bacteria enter your urinary tract.
Sexual Hygiene Practices

Building on these daily habits, specific practices around sexual activity provide additional protection. Pee before and after sex to help prevent bacterial problems. The before-sex urination helps empty your bladder, while the after-sex urination flushes out any bacteria that intercourse may have introduced. Some women also find that washing their genital area beforehand helps reduce bacteria, though this isn’t necessary for everyone. If you do wash, use gentle, plain water rather than soaps that can irritate sensitive tissues.
Products to Avoid and Use

Avoid douches, feminine sprays, and bubble baths. They can disrupt the protective bacteria in your vagina or irritate urethral tissues. These products can change your natural pH balance and make these infections more likely. What you wear and how you manage moisture also matter.
Choose cotton underwear instead of synthetic materials that trap moisture, and change out of wet swimsuits and workout clothes quickly. Consider sleeping without underwear for better air circulation. For menstrual products, replace tampons, pads, or menstrual cups every 4 to 6 hours. Pay attention to whether certain products seem to trigger episodes.
Read More: Women Who Start Menopause Before a Certain Age More Likely to Die Young
Natural Remedies For UTIs

Large studies with over 6,000 women showed that cranberry products reduce infection risk by 30% for women with frequent episodes. Cranberries contain compounds that create a slippery coating on bladder walls, making it harder for E. coli bacteria to attach and establish an infection. For best results, choose unsweetened cranberry juice, cranberry capsules, or dried cranberries, and focus on daily consistency rather than large occasional doses.
Other popular supplements don’t have the same proven track record. D-mannose gets attention online as a bacterial decoy. However, a large 2024 study of nearly 600 women found it no more effective than a sugar pill. Probiotics also lack solid evidence for preventing these infections despite theoretical benefits.
Say goodbye to recurring UTIs with Health First UTI Supreme! This triple-action formula features clinically proven Ellirose™ hibiscus extract, cranberry, and D-mannose to naturally support urinary tract health and prevent infections. With up to 89% reduction in recurrence over 6 months, you can finally get lasting relief. Take control of your health today!
When They Keep Returning

Doctors consider these infections recurrent when you get three in 12 months or two in 6 months. About 20% of women face this pattern, and many feel overwhelmed by it. Research into women’s experiences found that recurrent episodes leave many “feeling hopeless and helpless when it came to the management of their UTIs.”
These episodes can hurt social life, work, families, and relationships, often striking without warning. Recurring infections happen for two main reasons. Sometimes the same bacteria return by hiding in bladder tissues and emerging later, even after treatment. Other times, your anatomy, immune system, or daily habits make you vulnerable to new episodes.
Treatment for Frequent Episodes

Daily low-dose antibiotics for 6 months or more can break the cycle for many women with recurrent infections. The antibiotics stay in your urine at levels that keep bacteria from taking hold in your bladder without affecting your overall health. If these episodes follow sexual activity, your doctor might prescribe post-sex antibiotics to take within 2 hours of intercourse instead.
Many women worry about taking antibiotics long-term. Women understand the risks of bacteria developing resistance and know that antibiotics can disrupt the normal balance of good and bad bacteria throughout the body. Discussing these concerns with your doctor helps you weigh the benefits against the risks.
Pregnancy Concerns

During pregnancy, these infections need urgent attention because they become dangerous even without symptoms. Untreated bacteria can trigger premature labor, low birth weight, and serious kidney infections that threaten both mother and baby. Pregnancy makes this situation worse in several ways.
Hormones and physical changes make these infections both more likely and harder to detect. When left untreated, they progress to kidney involvement in 30% of pregnant women, compared to much lower rates in non-pregnant women. This is why doctors test urine for bacteria at every prenatal visit, treating even symptom-free cases.
Say goodbye to recurring UTIs with Health First UTI Supreme! This triple-action formula features clinically proven Ellirose™ hibiscus extract, cranberry, and D-mannose to naturally support urinary tract health and prevent infections. With up to 89% reduction in recurrence over 6 months, you can finally get lasting relief. Take control of your health today!
Menopause and Estrogen Changes

After menopause, these infections become much more common as dropping estrogen levels cause vaginal and urethral tissues to become thin and dry. The protective bacteria that depend on estrogen also decrease, leaving you more vulnerable to bacterial overgrowth. Fortunately, vaginal estrogen treatment can make a dramatic difference by restoring what menopause takes away. Studies show it reduces infection frequency from about 4 per year to less than 2. This treatment restores local hormone levels and tissue health without affecting the rest of your body like oral hormone therapy does.
Working with Specialists

Consider asking for a referral to a urologist or gynecologist if you get 3 or more episodes per year, keep getting them despite preventive antibiotics, or develop complications during pregnancy. These specialists can offer testing and treatments that go beyond what primary care doctors typically provide.
This includes cystoscopy to examine your bladder, imaging studies to check for anatomical problems, and advanced treatment options. Certain groups need specialist care even more urgently. People with diabetes, weakened immune systems, elderly adults, and pregnant women should seek immediate, aggressive treatment to prevent serious complications.
Building Your Prevention Plan

Track when episodes occur to spot your unique patterns and take targeted action rather than following generic advice. Work with your healthcare team during major life changes like starting birth control, pregnancy planning, or menopause. What prevents UTIs in your 20s might not work in your 50s. Stay flexible and communicate with providers about what’s working and what isn’t. These infections are incredibly common, and there’s no need to blame yourself for them.
Say goodbye to recurring UTIs with Health First UTI Supreme! This triple-action formula features clinically proven Ellirose™ hibiscus extract, cranberry, and D-mannose to naturally support urinary tract health and prevent infections. With up to 89% reduction in recurrence over 6 months, you can finally get lasting relief. Take control of your health today!
Read More: 10 Simple Remedies to Help Relieve Gum Disease At Home
Disclaimer: This information is not intended to be a substitute for professional medical advice, diagnosis or treatment and is for information only. Always seek the advice of your physician or another qualified health provider with any questions about your medical condition and/or current medication. Do not disregard professional medical advice or delay seeking advice or treatment because of something you have read here.
